Switch to the mobile version of this page.
Vermont's Independent Voice
- News
- Arts+Culture
- Home+Design
- Food
- Cannabis
- Music
- On Screen
- Events
- Jobs
- Obituaries
- Classifieds
- Personals
Browse News
Departments
-
Housing Crisis

Barre to Sell Two Parking Lots for…
-
News

Vermont Awarded $62 Million in Federal Solar…
-
News

Property Tax Relief Bill Sparks Partisan Feud
- Town of Roxbury Sues Over Budget Vote That Could Close Its School Education 0
- More Vermont Seniors Are Working, Due to Financial Need or Choice. They May Help Plug the Labor Gap. This Old State 0
- Burlington Mayor Emma Mulvaney-Stanak’s First Term Starts With Major Staffing and Spending Decisions Politics 0
Browse Arts + Culture
View All
local resources
Browse Food + Drink
View All
Browse Cannabis
View All
-
Culture

'Cannasations' Podcaster Kris Brown Aims to 'Humanize'…
-
True 802

A Burlington Cannabis Shop Plans to Host…
-
Business

Judge Tosses Burlington Cannabiz Owner's Lawsuit
-
Health + Fitness

Vermont's Cannabis Nurse Hotline Answers Health Questions…
-
Business

Waterbury Couple Buy Rare Vermont Cannabis License
Browse Music
View All
Browse On Screen
Browse Events
View All
Quick Links
Browse Classifieds
Browse Personals
-

If you're looking for "I Spys," dating or LTRs, this is your scene.
View Profiles
Special Reports
Pubs+More
Published April 25, 2018 at 10:00 a.m. | Updated December 23, 2018 at 2:07 p.m.
Francis offered up a stuffed Yoshi toy and a Coke as he poked his head into a white-walled room last August at Brattleboro Retreat.
He found his son, Simon, sitting hunched over on a hospital bed. Instead of greeting his dad, the 22-year-old patient glared menacingly at the man who had just driven two and a half hours from Burlington to see him. Then Simon got up and silently snatched the beverage — 24 ounces, no ice — before retreating to his former spot in the back corner of his mattress.
It had been 23 days since Simon was admitted — against his will — to the psychiatric hospital. During that time, he had consumed only Coke and milk. His clothes hung from his emaciated limbs; his sandy hair stood on end. He could no longer hold a conversation or manage his personal hygiene. He also had refused to take his medication — the one thing that doctors said could improve his condition.
He was at Brattleboro for psychosis — his second "episode" since puberty. Delaying drug treatment could put him at greater risk of permanent neurological damage.
Francis made small talk, trying to entice his son to drink milk through a straw or to play with the toy.
Simon responded with a stream of gibberish punctuated by occasional, intelligible profanity: "Nazi," and later, "I'm going to fuck you like Kim Jong-un."
"He didn't used to be a swearer," Francis observed with resignation. Dad kept his cool, too, when Simon got up to spin in place for a few minutes.
Francis showed more emotion on the drive home. When Simon was first hospitalized, he said, he'd wait until he was out of the building before breaking down. "Now, I'm just numb," he said with a sigh.
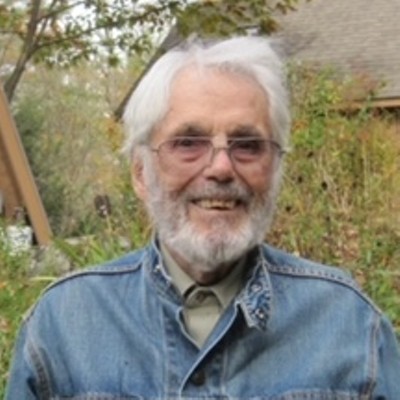
Meeting his own needs has been challenging, said Francis, who requested anonymity for his son. To protect Simon's privacy, Seven Days also assigned pseudonyms to his relatives quoted in this story. "I've been there for Simon," said Francis, "but it's been very difficult to take care of myself."
Francis is one of 6,562 Vermonters living with and caring for a family member with an intellectual or developmental disability: Simon has a genetic condition and is autistic. He also has a co-occurring mental illness — schizophrenia.
That means, in addition to being an unpaid, 24-7 nursing aide, Francis has to figure out which of Vermont's myriad community-based programs, from case management to respite, might help his son. Gov. Phil Scott's recently proposed $4.3 million cut to the Developmental Disabilities Services Division would potentially curtail or eliminate some of them.
Inpatient hospital care poses a different set of challenges. Since the state mental hospital in Waterbury closed in 2011, Vermont hasn't had enough beds to accommodate patients suffering from acute mental illness.
Simon spent three days in the emergency room at the University of Vermont Medical Center before he was sent to Brattleboro — in spite of his dad's request to keep his son in Burlington. Francis made the 150-mile trip two or three times a week to southern Vermont while Simon was hospitalized there.
Despite his dedication, Francis, 64, has no say in his adult son's treatment. Vermont has some of the most protective patients' rights laws in the country, which, along with federal health care privacy laws, prevent family members from participating in the legal proceedings that determine what happens to their loved ones in the hospital.
That leaves parents with few options — and typically, weeks of waiting — while their son or daughter is unable to make decisions about his or her care, including medication.
"Simon thinks he's on a spaceship," his father said. Meanwhile, "they're treating Simon like he can advocate for himself."
Francis watched helplessly as Simon lay incapacitated for three and a half months in Brattleboro and two more at the UVM Medical Center. But he channeled his powerlessness into research and lobbying for his son's forced medication. From his Burlington apartment, he spent long hours investigating Vermont's mental health laws. He called every state senator in Chittenden County, the governor's office and Seven Days to make his case.
After two decades molding his life around the needs of his son, Francis summed up his frustration: "I think the greatest suffering is to look on someone and be able to do nothing."
Raising Simon
Simon's problems can be traced to a genetic disorder called 22q11.2 deletion syndrome, caused by a defect in the 22nd chromosome. The abnormality increases the likelihood of adolescent-onset mental illness. And it can cause a range of physical problems, from cleft palate to breathing troubles. For Simon it resulted in a weak immune system, learning disabilities and distinctive facial features: almond-shaped eyes and a wide nose.
It also left Simon with life-threatening congenital heart defects. Specifically, he was born with a hole between his right and left ventricles and a left pulmonary artery made of temporary tissue — rather than permanent tissue — that got reabsorbed by the body.
Simon was 3 days old when doctors sent him via medevac helicopter to Boston for his first open-heart surgery. "Don't be surprised if you get there and he's dead," Francis recalled the physicians saying.
"His introduction to life was basically that he had PTSD since before he was verbal," Francis said. "And no sooner did he recover from one surgery when he had another."
For post-op pain, baby Simon got morphine and quickly developed a dependence on it. Within weeks of his birth, he was on methadone. His parents weren't allowed to pick him up until he was 1 month old.
Both of them had experience with kids with disabilities. Simon's mother, Kim, worked as a speech and language pathologist, and Francis taught preschool for low-income and at-risk kids.
Growing up in Barton, Simon exhibited "a lot of eccentricities," according to his older sister, Joy. But he liked books and video games. Together they played with Matchbox cars or went to the river near their house.
As a teenager, Simon got interested in aviation. He took nearly 20 flight lessons in Newport until he could take off and fly by himself; he studied the handbook and hoped to earn his pilot's license.
Nonetheless, Simon's health issues took a toll on the family. By the time he was 12, Simon had undergone two more open-heart procedures. To date he's had 15 cardiac catheterizations.
Another of his physical problems — a perforated velum, the membrane that keeps food from coming out of the nose — made mealtimes tense, Joy recalled. Simon vomited often.
"It was all hands on deck," his sister continued, suggesting her parents stayed together to "help raise Simon." Kim and Francis separated five years ago. Simon's mom did not respond to multiple interview requests.
At 15, Simon started having occasional delusions, and doctors put him on Risperdal for psychosis and the antianxiety drug Ativan. But Simon worried that his medications were making him see things and stopped taking them, and his symptoms worsened.
At one point, he was convinced that a stick in the yard was the government, watching his every move, Joy recalled.
He was diagnosed with schizophrenia and spent 10 days in isolation at Brattleboro Retreat, Francis said. That time, involuntary medication wasn't necessary; Simon was lucid enough to be convinced that he wouldn't be able to leave the hospital unless he took his medication.
But the experience left him with decreased cognitive function and a lasting fear of Brattleboro Retreat, Francis said. He stopped taking flight lessons. He could no longer get through an entire novel. Although he graduated from Lake Region Union High School in 2014, he "didn't have the skills of a high school graduate," Francis said.
For seven years after his diagnosis, Simon dutifully took the medications he was prescribed. In October 2016, he moved to Burlington for the social services — psychiatry and job training opportunities — offered in the Queen City.
He lived alone in an Old North End apartment, ordering in or microwaving his food, doing his laundry and taking the bus where he wanted to go — typically Walmart, the airport to watch the planes, and the University Mall. He set up his own appointments with his psychiatrist.
Francis visited on weekends, when he'd clean the apartment and buy groceries for the coming week.
He made reminders on index cards and provided cash rewards to motivate Simon in his absence. Simon got $1 for brushing his teeth, taking a shower or eating a banana each day. He earned $5 for larger successes, such as making it to therapy on time or going somewhere new on the bus.
Soft-spoken Francis has been in counseling since Simon was a baby. He meditates daily, does yoga and attributes his sanity to Buddhist-Christian "spiritual work." But after nine months spending every weekend in Burlington, he was "worn out." He decided to retire early from North Country Supervisory Union, and last June he relocated to Burlington to live with his son. One wall of the apartment's living room is now lined with Francis' books on philosophy and religion; the other side features Simon's collection of Matchbox cars.
Francis said he was relieved to leave the Northeast Kingdom. He said he never fit in there and has since dyed his hair blue.
Another reason for the move: Francis knew that his son was likely to have another psychotic episode.
All in the Family
Vermont family members didn't always function as de facto caretakers for people with developmental disabilities. For decades, the Brandon Training School housed as many as 600 such individuals.
In 1978, Vermont Legal Aid filed a class action lawsuit on behalf of one resident, Robert Brace, who wanted to move out of the facility. The settlement agreement, called the Brace Decree, created a 10-year plan to move hundreds of residents out of the institution and into the community.
The school closed in 1993.
In 2002, the state shuttered its last sheltered workshop, which employed adults with physical or mental disabilities separately from the rest of the population.
By the early 2000s, the Vermont State Hospital in Waterbury, which housed Vermonters with mental illness, was also on its way out. The building, constructed in the 1890s, was decrepit, and in 2003, two patient suicides and a series of complaints about care led federal authorities to decertify the hospital. That meant that it could no longer care for Medicare- and Medicaid-eligible patients — a loss of $9 million in annual revenue.
The hospital closed for good in 2011, after Tropical Storm Irene swept through and destroyed the building.
The result? Community-based care has provided more autonomy and greater integration for those with disabilities — an approach for which Vermont has won accolades.
The downside: There's more pressure on families to help their loved ones find the services they need.
The burden was heavy for single mom Lynne Cleveland Vitzthum, a former state rep and staffer for Sen. Patrick Leahy (D-Vt.). She said her son, who has autism and cerebral palsy, was among the first in Vermont to be mainstreamed.
But she discovered she was responsible for finding state services and fighting to keep him integrated in public school. When state support didn't materialize, she got involved in politics to address the inequities herself. Parents "have to be the lead advocate for their child," said Vitzthum, who now works as developmental disability services director for Vermont Care Partners.
Similarly, those who answer the parent hotline at the Vermont Family Network, an organization for families of children with special needs, get questions about how to deal with a child's mental health or behavioral issues, navigating the medical system, and what state money might be available to them, said Lisa Maynes, a family support director for the organization.
"It's hard for families to know what the system is and what they might want to ask," Maynes said. "The burden on families and individuals to advocate for themselves and be aware is just getting bigger."
It's not unusual for someone to call the hotline exhausted or crying, just looking for someone to listen. The stress is "physical, emotional, financial," Maynes said.
More often than not, the state does not provide what they seek.
To take deinstitutionalization seriously, "we do need to fund robust community support and family support," said Kirsten Murphy, director of the Vermont Developmental Disabilities Council, a statewide advocacy board. "In the case of family support, I'm not sure we ever did."
Murphy said she raised her son, who has developmental disabilities, in New Hampshire, where a separate line item in the state budget generously funds family caregivers. In contrast, in Vermont, Gov. Scott is proposing a 2 percent cut, totaling $4.3 million in state and federal funding, to services for Vermonters with disabilities. If the legislature approves the changes, the Developmental Disabilities Services Division for the State of Vermont program would trim or eliminate employment supports, community programs and respite funding, according to Clare McFadden, the division's director.
Ron, who also asked for anonymity, said he could have used a lot more help in the six years he spent managing the care for his schizophrenic son, who's now 27.
At one point, his son fled from a group home. Six months later, he called from Philadelphia, asking for a ride home. Another time, he told Ron's wife that he had considered slitting her throat. "You feel like a prisoner in your own house," Ron said.
Things improved only when Ron found his son a subsidized apartment in downtown Burlington and told him to move out.
The difference came in "knowing that you have a safe haven ... and your loved one has some other place," he said. That cut the stress "by two-thirds."
During those trying days, Ron found a community in the support groups hosted by the Vermont chapter of the National Alliance on Mental Illness. In conversations with other parents, he found he wasn't alone. They echoed the sense of isolation, the stress, the feeling of helplessness that Francis, too, describes.
Among parents, those sentiments "are across the board," said Ron.
Simon's Slide
Simon's second psychotic episode started about a month after Francis moved in with him in Burlington. While Francis was at yoga class, his son took a flight through space, he told his father; Simon had arrived back safely, he said, but had turned off the fans and closed the windows in the house to help with the landing.
In the following days, Simon started refusing to take his medication, reasoning that it was causing him to lose touch with reality.
As he drifted further into an alternate universe, Simon noted that his copilot was pop singer Demi Lovato.
Francis took detailed notes of Simon's jumbled monologues. His son rambled about hypersonic aircraft, his preference for Windows 7, Selena Gomez and aliens.
On August 3, Simon became unruly and Francis called the Burlington Police Department to transport him to the UVM Medical Center.
A psychiatrist evaluated him within 24 hours of his arrival, as is required for involuntary admissions, but Simon waited three days in the emergency room for a mental health bed to open up.
Brattleboro Retreat offered to take him, and doctors there started the legal process that would allow them to hospitalize Simon without his permission.
A lawyer from the Vermont Attorney General's Office filed a petition on behalf of the Department of Mental Health — and the doctors at Brattleboro Retreat — asking a judge to rule that the hospital could hold Simon for 90 days.
The state also filed a separate petition to medicate Simon.
The court hearing for both matters was scheduled for September 8, a month and a day after he was first admitted; meanwhile, Simon, who had refused medication, became sicker.
He spent weeks sitting on his bed while a psych tech manned a desk outside his room. Simon refused to eat and soiled himself repeatedly. He allowed a staff member to brush his teeth just once.
He growled or cursed at staff members and, sometimes, hit or kicked them. They had to subdue him a few times — with a cocktail of antipsychotic and antianxiety drugs, plus Benadryl — in order to clean him up. Francis and Kim alternated driving down to visit: he from Burlington; she from Barton, which is a three-and-a-half-hour drive.
Francis attributed some of Simon's disorderliness to withdrawal from Ativan, which he had been taking for seven years. Abruptly quitting the drug can cause severe withdrawal symptoms, including poor sleep, agitation, mental jolts and anxiety, according to Dr. Sandra Steingard, chief medical officer for the Howard Center.
A lack of treatment for psychotic patients can also slow the healing process or cause permanent brain damage, said Dr. Robert Pierattini, chief of psychiatry at the UVM Medical Center.
That's what motivated Francis to spend hours on the phone with nonprofits, legislators and hospitals in an effort to force his son to take his drugs.
But his lobbying efforts haven't persuaded Jack McCullough, director of Vermont Legal Aid's Mental Health Project, who said he regularly hears from parents who think it's clear that their son or daughter should be hospitalized and medicated.
McCullough called involuntary medication "a serious deprivation of liberties."
"Of all the players in the system — the psychiatrist, the social worker, the judges, the Department of Mental Health — everyone else in the process is there to try to figure out what the client needs. We're the only element in the system that's there to stand up for what the client wants," McCullough said. "I make no apology for standing up in court to assert that. It's what any of us would want."
'Thy Will'
A relatively small number of patients in Vermont — about 70 a year — are medicated involuntarily, most commonly for schizophrenia and manic iteration of bipolar disorder, according to Dr. Mark McGee, chief medical officer for Brattleboro Retreat. McGee said he has long advocated for a more efficient process to pursue medication — and more authority for doctors, rather than judges.
In 2014, the legislature voted to streamline the judicial process and allow the option of expedited hearings for those seeking involuntary medication.
According to advocates on both sides, the emotional testimonies and jammed committee hearings made some legislators reluctant to take up the issue again.
Even after the changes, though, the process typically takes weeks; last year the average time between hospitalization and a court date was 62 days.
Simon's expedited hearing was scheduled in half that time — due in part, perhaps, to his dad's advocacy.
Francis was barred from the September 8 proceedings in Windham County Family Court, except to testify briefly on his son's condition. Nor was he allowed to speak with Simon's lawyer, awarded by Vermont Legal Aid.
In the end, Judge Katherine Hayes granted the involuntary medication order, as the state does in about 80 percent of such cases. Simon received a shot of antipsychotic medication that day and promptly wolfed down his first solid food in five weeks, his father said.
Still, healing was gradual.
Simon stayed in Brattleboro, where he refused all food except McDonald's. Francis continued his visits but gave up hope of changing the involuntary medication laws. "I just ran out of energy," he said.
Simon didn't notice when he turned 23 on September 27. Francis headed down to celebrate anyway.
He and Kim briefly considered petitioning for legal guardianship of their son; Simon's second psychotic episode suggests the increased likelihood of a third — and a fourth, according to Steingard.
Ultimately, though, they decided against it. Simon's parents were unwilling to pursue the lengthy and expensive process, and even as guardians, they wouldn't have the right to grant permission for involuntary medication in the case of another psychotic breakdown.
"It wouldn't have given us any more control," Francis concluded.
On November 17, after more than three months at Brattleboro Retreat, Simon developed what looked like congestive heart failure. The doctors medevacked him to the UVM Medical Center.
Almost a month later in the Burlington hospital, Simon was in better shape physically but still psychotic. He paced around his bed mumbling, hair tangled and unruly, and warned his father about the Borg, a fictional alien group featured in "Star Trek."
He referred to this reporter as Katy Perry. On the whiteboard, after the nurse's name "Hannah," he had written "Montana" in a large, childish scrawl.
At one point, a nurse came in to fix Simon's bed alarm; he tried to grab the RN, ordered him out of the room and cursed him violently.
Francis responded by suggesting he and his son "snuggle." He lay down alongside Simon in the hospital bed, his arm around his shoulders. Simon slowly relaxed, his invectives grew silent, and he laid his head on his father's chest.
Sometimes, Francis stayed on the hospital bed for an hour or more, he explained later. Often, he prayed. He repeated a single invocation: "Thy will be done." It's "a coming to terms with the fact that I have no power," he said. "There's nothing I can do about this."
Home Again
On January 15, Simon returned to his apartment in Burlington.
That wasn't the plan: Doctors at the UVM Medical Center had tried to find him a high-security bed at every mental hospital in Vermont, as well as a few out of state, Francis said. None would take him, because of his past violence with staff, reluctance to take his meds and complicated medical history.
Instead, Simon moved back in with Francis, who remains his unpaid, 24-7 caregiver.
The stress level "is back to how it was when he was 4 or 5," Francis said, "except now he's an adult."
Nonetheless, Francis is convinced "it's the best-case scenario" and that if Simon had stayed in the hospital, he would have backslid and returned to his previous state of psychosis.
Simon sleeps about 18 hours a day, likely because he's on four meds: the antipsychotics Haldol and Zyprexa and the antianxiety drugs Phenobarbital and Valium.
Most days, Simon wakes at 8 a.m. to take his medication, then goes back to bed. He gets up for lunch — usually grilled cheese or a McDonald's burger. His favorite afternoon activity is accompanying Francis to the grocery store or to his South End art studio. While Francis paints vividly colored designs, creating "order out of chaos," Simon sits in the car and watches people in the parking lot.
Francis celebrates the small victories: the February day Simon opened a can of soda on his own; the time he started to dress himself.
A bigger one: The son finally gave his father written permission to access his medical records — Francis hadn't been able to get that information since Simon turned 18.
The day before Town Meeting, Francis recalled, Simon engaged in his first full conversation since he was admitted to the hospital last August. He expressed interest in voting — for independent mayoral candidate Carina Driscoll — then decided against it.
On April 5, Simon paged through Motor Trend, his favorite car magazine, looking at the pictures. And on the 12th, he put his clothes in the dryer on his own.
Later that same day, Simon lay on his side on the bed, raising his head only to express how much he dislikes his father's Amazon Echo.
When this reporter started to make small talk, he turned away. "You talk to her," he told his father.
Simon receives Medicaid waiver funding, which can be used to pay friends and neighbors to care for him and provide his father a respite. But for now, Simon refuses to spend time with anyone other than his father.
Finances are tight. Francis gets $780 monthly from Simon's disability insurance, about half the cost of his care, he said. Otherwise, he lives off his teaching pension.
He breathed a sigh of relief when he confirmed that Simon's Medicaid and the State of Vermont covered what Francis estimated to be $500,000 in hospital bills.
But he worries constantly about Simon; the median lifespan for someone with his condition is 29 years. "I've always thought I was going to bury my son," Francis confessed.
Her parents had always assumed that Simon would be independent, Joy said. The prospect of caring for him long-term or finding an alternative solution? "I don't think they ever really saw it coming," she said.
Francis occasionally warns Simon that he won't be around forever, either; the prospect of having to find another caregiver would mean navigating "another world of social services that I have absolutely no faith in," Francis said.
But Simon's not worried about his father's death. According to Francis, they'll address that challenge as it comes — just like they've faced every one before this.
"I'm not going to give up," said Francis. "I don't have any other option. And neither does Simon."
Related Stories
Got something to say?
Send a letter to the editor
and we'll publish your feedback in print!
Tags: Health Care, mental health, mental illness, psychosis, schizophrenia, developmental disability, intellectual disability
More By This Author
Speaking of...
-

Rep. Anne Donahue Is Determined to Find Out Where Patients of Vermont’s Old Psychiatric Hospital Are Buried
Mar 20, 2024 -

Noah's Arc: Noah Kahan Is Vermont's Biggest Cultural Export in Years. How the Hell Did That Happen?
Jan 31, 2024 -

Vermont Colleges School Students on Wellness as Mental Health Concerns Mount
Jan 17, 2024 -

A Young Man's Path Through the Mental Health Care System Led to Prison — and a Fatal Encounter
Sep 6, 2023 -

Two School Districts Create Their Own Programs for Students With Special Needs
Sep 6, 2023 - More »
Comments (12)
Showing 1-10 of 12
Comments are closed.
From 2014-2020, Seven Days allowed readers to comment on all stories posted on our website. While we've appreciated the suggestions and insights, right now Seven Days is prioritizing our core mission — producing high-quality, responsible local journalism — over moderating online debates between readers.
To criticize, correct or praise our reporting, please send us a letter to the editor or send us a tip. We’ll check it out and report the results.
Online comments may return when we have better tech tools for managing them. Thanks for reading.
- 1. Barre to Sell Two Parking Lots for $1 to Housing Developer Housing Crisis
- 2. Vermont Awarded $62 Million in Federal Solar Incentives News
- 3. Home Is Where the Target Is: Suburban SoBu Builds a Downtown Neighborhood Real Estate
- 4. More Vermont Seniors Are Working, Due to Financial Need or Choice. They May Help Plug the Labor Gap. This Old State
- 5. Property Tax Relief Bill Sparks Partisan Feud News
- 6. Burlington Mayor Emma Mulvaney-Stanak’s First Term Starts With Major Staffing and Spending Decisions Politics
- 7. Town of Roxbury Sues Over Budget Vote That Could Close Its School Education
- 1. Totally Transfixed: A Rare Eclipse on a Bluebird Day Dazzled Crowds in Northern Vermont 2024 Solar Eclipse
- 2. Zoie Saunders, Gov. Scott’s Pick for Education Secretary, Faces Questions About Her Qualifications Education
- 3. Don't Trash Those Solar Eclipse Glasses! Groups Collect Them to Be Reused 2024 Solar Eclipse
- 4. Burlington City Council Approves Rezoning Plan to Boost Housing Supply News
- 5. State Will Build Secure Juvenile Treatment Center in Vergennes News
- 6. Rising Costs and Property Tax Hikes Again Threaten the Survival of Small Schools Education
- 7. Queen of the City: Mulvaney-Stanak Sworn In as Burlington Mayor News